One of the biggest discoveries in medical research today is that experts are finding solid links between health conditions a person is affected by and their resulting susceptibility to future decline of cognitive function.
In the past, cognitive decline was primarily associated with the aging process, but it is becoming increasingly clear that certain illnesses are having significant impact on how soon that decline may begin.
Yes, researchers are seeing predictability in what is leading to the loss of cognitive function.
Most importantly, our yet-unaffected population still has time to make a positive difference in their cognitive health destiny. Remarkable indeed. We now hold the key to the future. This is a game-changer.
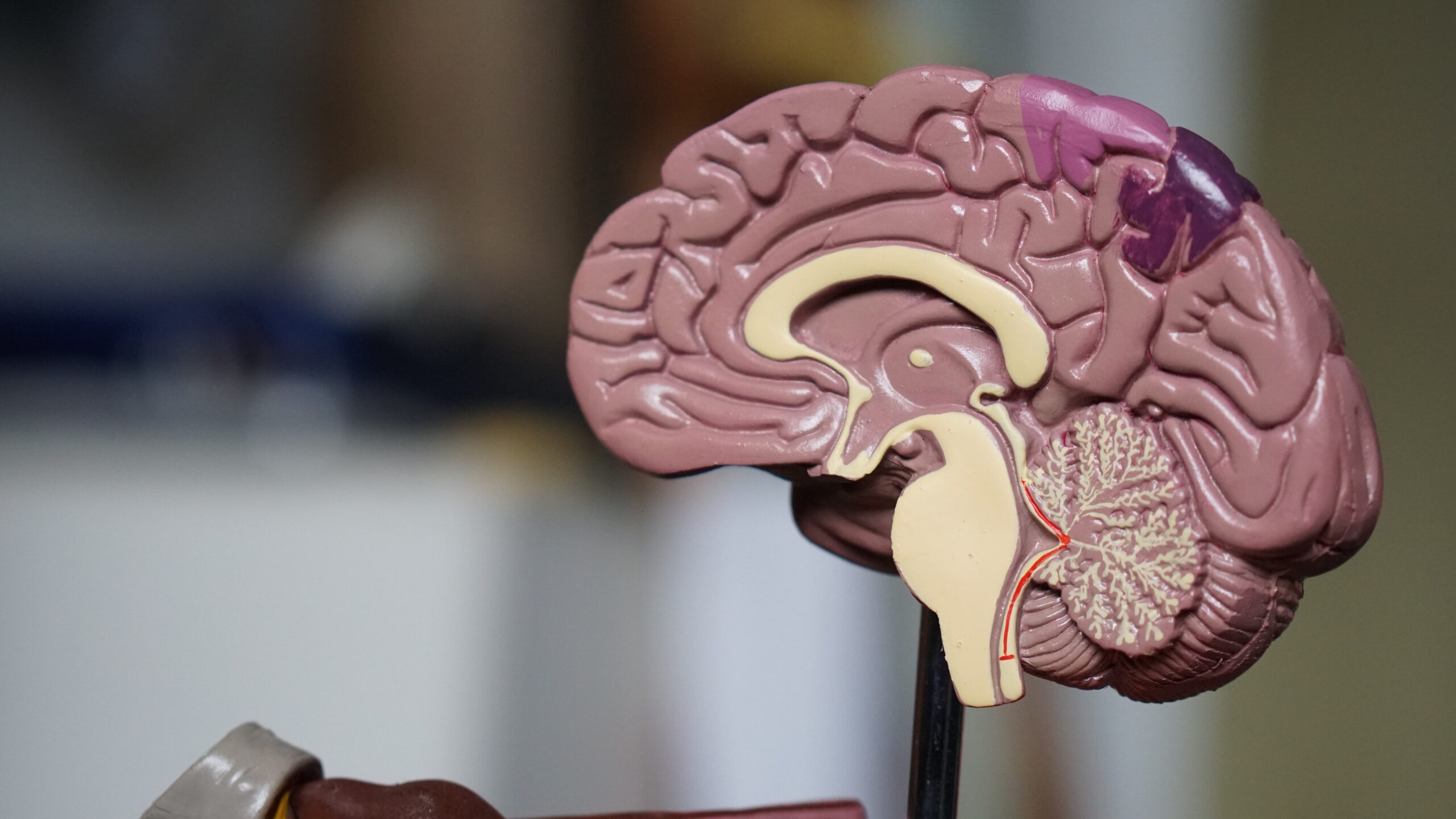
First, it’s important to understand what cognitive function is. It is a human’s working composition of mental abilities and their capability to process information. This includes the ability to acquire knowledge, process it, remember it, concentrate on it, reach a decision, and more. It has many variables and is akin to an intricate web.
Explaining the vital data that has been gleaned recently is internationally-recognized expert Dr. Richard Lipton, principal investigator of the Einstein Aging Study.
Lipton’s credentials include being the Edwin S. Lowe Professor and Vice Chair of Neurology, Professor of Epidemiology and Population Health, and Professor of Psychiatry and Behavioral Science at the Albert Einstein College of Medicine.
The Einstein Aging Study (EAS) was developed to focus on the aging brain, to examine both the normal aging process and the special challenges of Alzheimer’s disease and other dementing disorders.
The goals of the study are as follows*:
- Describe the changes in memory and thinking which occur in normal aging.
- Develop tests which help identify early Alzheimer’s disease and individuals at high risk for future disease.
- Study the causes of Alzheimer’s disease.
- Discover the changes in the brain which cause memory loss and other cognitive symptoms.
- Devise treatment strategies which delay or reverse brain changes.
- Provide education and information to EAS participants and the community about the aging brain.
The study is conducted via comprehensive testing.
“What’s unique about EAS is that we do a lot of ambulatory assessments,” Lipton said. “We measure cognition using tests that are given on a smartphone. They are very brief tests and are given six times a day for 14 days.”
In order for the best, most invasive results if you will, Lipton explained, “The advantage of doing [multiple assessments] is that we know that cognitive performance varies within a person from moment-to-moment and day-to-day.”
One thing Lipton underscored is that “cognitive ability doesn’t vary at random.”
His prime, relatable examples of that include, if a person:
- “Has a bad night’s sleep;
- Is diabetic and their glucose is out of control;
- Is in an environment with a high level of air pollution;
- Is under stress.”
Lipton emphasized that all of these have the ability to influence cognitive performance.
“EAS measures all of those things and we look at risk factors for short-term decrements in cognitive performance linked to sleep, pain, diabetes regulation, or air pollution,” Lipton said. “It turns out that vulnerability to environmental stressors and variability in cognitive performance are in and of themselves predictors of cognitive decline. That gives us better estimates of how [individuals are] doing on the average.”
It might benefit all of us to take a few moments to reflect on the inconsistencies we have experienced over the past 72 hours: our mood variances, lessening or strengthening of chronic pain throughout the body, stress levels, shifts in alertness, feelings of anxiety, and general wellbeing. When self-analyzing, it really underscores that EAS is set up to conclude the most accurate, well-balanced results.
EAS was developed for the benefit of humanity as a whole. It is an evolving toolbox for both experts to better understand the human brain to further medical science, and for us, as individuals, who also hope for education and findings that promote healthier aging, with the hope of delaying or mitigating decline in cognitive function.
Lipton said EAS shows, “How much [individuals] are changing on average, but also factors that may influence short term cognitive variability and long term cognitive decline.”
When asked if a correlation between age and decline in cognitive function still holds merit, he said, “We know that broadly speaking, certain kinds of cognitive performance decline with age in virtually everyone and we call that normative cognitive decline.”
“We also know that a lot of cognitive decline in older adults is related to illness,” he continued.

Lipton noted that cognitive decline is related to the onset of Alzheimer’s disease. “Our study and others have shown, for example, that when people are on the road to Alzheimer’s disease, memory decline accelerates seven years before diagnosis. Executive function – the ability to plan – begins to decline about three years before diagnosis.”
An additional significant discovery has been that stress has a tremendous impact on future cognitive function.
To be blunt, how you deal with stress in your life will affect your future wellbeing. We know that high levels of stress can have physical ramifications like high blood pressure, etc., but who knew it can truly lead to early cognitive decline?
Stress is inherent in our lives. Our individual stressors can be very different, as well as very relatable. How we individually process stress, work through it, and consciously reduce it may become more of a priority after understanding its relationship to our future.
“Stress plays a very important role and it’s an issue that a lot of people study,” Lipton said.
“Our group has shown that individuals who have a high level of perceived stress develop cognitive decline, mild cognitive impairment and dementia at higher rates than people who have lower levels of stress,” he said.
“People do much worse following a high-stress day than they do following a low-stress day, and the magnitude of that effect is equivalent to about four years of normal aging,” Lipton said.
We’ve heard stress isn’t good for us; we just didn’t know how truly treacherous it is.
The interrelationship between stress and cognitive function is not to be taken lightly. These findings are alarming.
Now is the time for all of us to find stress-relieving tools tailored to our unique needs. Our healthy mental function is dependent on it.
Most of us have seen how stroke often impairs cognitive function. “We know a very common cause of dementia in older adults is actually the development of multiple strokes and that’s a condition that gets called vascular dementia,” Lipton explained.
There are many variables and conditions that can serve as risk factors for stroke.
“There are many pathways that contribute to damage to the brain that can lead to cognitive decline and ultimately to dementia; migraine with aura is one of the vascular risk factors that can lead to cognitive decline,” said Lipton. “We know that there’s a link between the frequency of attacks of migraine with aura and the risk of having either clinical strokes or even subclinical strokes that you can see on an MRI.” (A subclinical stroke can be described as a ‘silent stroke’ where there are no outward symptoms but brain lesions are seen in imaging.)

Thus far, we know illness, stress, migraine and stroke have been linked to the decline of cognitive function. An additional major discovery in this category has been the impact of chronic pain.
The number of individuals living with chronic pain in our population is immense. Many of those have developed a high tolerance to it. Quite a number downplay it and just endure it, year after year.
According to Lipton, “Half of older adults meet the International Association for the Study of Pain criteria for chronic pain.”
Chronic pain can be defined as pain that is consistent or comes/goes for over three months. It impacts the quality of life of a person as it interferes with daily activities.
“We know that if you have chronic pain that’s bad enough to interfere with daily function, [it] is a predictor of incident dementia,” Lipton said. There are plethora of illnesses and diseases that co-exist with chronic pain.
“People with chronic pain are actually more likely to develop dementia than people who don’t have chronic pain and that follows and parallels in some ways the findings that say, migraine, in particular migraine with aura, is a risk factor for cognitive decline and dementia as well,” Lipton said.
Given we now have this information thanks to Dr. Lipton and the Einstein Aging Study, how can we use it to our advantage?
If you are suffering from stress, chronic pain, migraine, or illness, commit to finding a doctor who is qualified to give you an accurate medical diagnosis and recommend viable and successful treatment options that are available for your condition.
In addition to finding a better quality of life with the right treatment plan, taking positive action and collaborating with your doctor can help preserve your long-term cognitive health.
Never has there been a more opportune time to be steadfast in improving your overall health.
In epidemiology, Lipton said, “You want to find modifiable risk factors to protect people against the consequences of those risk factors.”
“For example, if we know hypertension is a risk factor for stroke and dementia, we want to treat hypertension; we want to control hypertension to reduce the effects” of less-than-desirable outcomes.
As we know, it may take time to find the right doctor, therapist, or treatment modality. Being proactive and continuing to seek a medical professional that leads us to a successful result is what must take priority. We have a lot at stake.
Given the valuable information that has been learned thus far through the Einstein Aging Study, which began in 1980, it is gratifying to learn that it has just been refunded for another five years. It is certain we can look forward to more promising findings from it.
Dr. Richard Lipton’s research has included population studies that link stress, pain and cognitive performance to genetics, biomarkers, and neuroimaging. Through EAS, he has focused on cognitive aging across the lifespan with emphasis on the effects of pain and stress on brain function.
A highly-respected headache researcher who focuses on migraine, Dr. Lipton is a five-time winner of the H.G. Wolff Award for excellence in headache research from the American Headache Society and a two-time winner of the Enrico Greppi Award from the European Headache Foundation.
Dr. Lipton is the Chair of the Scientific Advisory Board at Biohaven Pharmaceuticals.
*https://www.einsteinmed.edu/departments/neurology/clinical-research-program/eas/
Coming next: Migraine still widely under-diagnosed, expert says
Dr. Lipton’s contribution to our society is immense.