COPD, formally known as Chronic Obstructive Pulmonary Disease, is the fourth leading cause of death and a major cause of disability in the United States, according to the National Heart, Lung, and Blood Institute.
This is a disease that deserves a look back in time as a lot has changed and evolved with it. COPD is one of many conditions that has been studied over time and what has been learned historically has led to better treatments, understanding, and management of the disease.
The Centers for Disease Control and Prevention (CDC) defines COPD as “a group of diseases that cause airflow blockage and breathing-related problems. It includes emphysema and chronic bronchitis.” While no cure is available for COPD, it is treatable.
Columbia University has stated “over 15 million Americans have been diagnosed with COPD. Evidence suggests that another 15 million have COPD but remain undiagnosed.”*
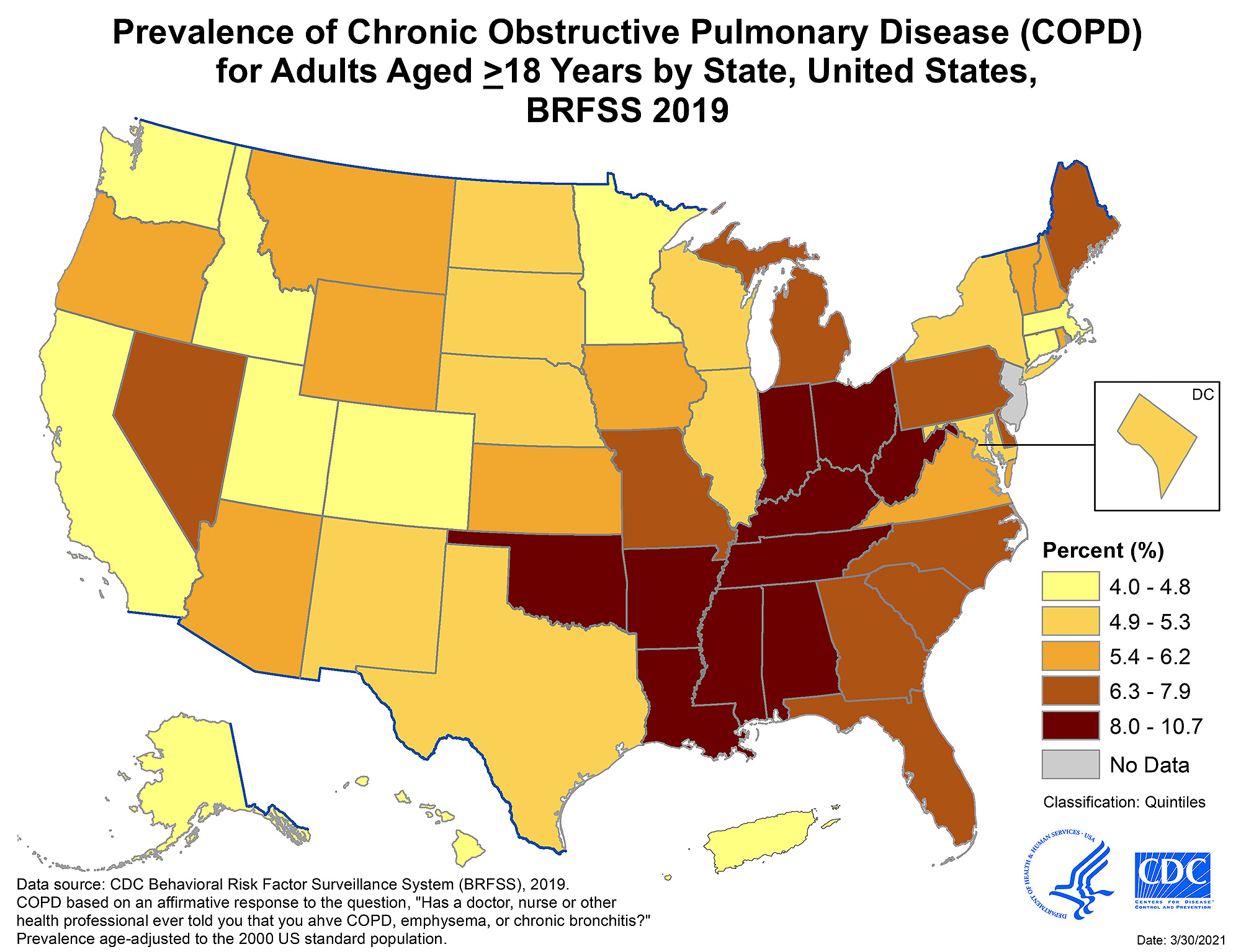
The CDC’s chart within this post depicts the locations of “hot pockets” (or areas of most prevalence) of COPD sufferers in the United States.
It is important to understand that there are various conditions housed under the name COPD. In other words, “all COPD is not the same.”*
Some individuals have a chronic bronchitis form of COPD; others have a more emphysematous form (related to emphysema).
Emphysema “is a progressive, destructive lung disease in which the walls between the tiny air sacs are damaged.”* In turn, breathing becomes difficult due to the lungs’ loss of elasticity and air becomes trapped in the person’s over-inflated lungs.
While most cases of COPD are linked to a history of smoking, 25% of patients diagnosed with the condition have never smoked.
Something everyone should understand is that research has pointed to environmental factors playing a role in developing and enhancing symptoms of COPD. One genetic form is known called alpha-1 antitrypsin deficiency.
A notable turning point globally came as a result of the 1952 Great Smog of London, which tied together respiratory death and impaired air quality. Studies and research ensued.
The event was described as follows. On December 5, 1952, a yellow-brown smog encased London, wreaking havoc on citizens and it quickly led to a crisis.
The poisonous and paralyzing smog, which lasted for five days, was caused by a toxic mix of industrial pollution (soot from factory smokestacks, automobiles, chimneys, and diesel-fueled buses) and high-pressure conditions (causing a temperature inversion).
It is estimated that around 12,000 lives were lost because of the Great Smog of London. “Deaths from bronchitis and pneumonia increased more than sevenfold. The death rate in London’s East End increased ninefold.”***
The smog was so thick that some residents were unable to see their feet as they walked. I’ve touched on the impact of air pollution and migraine but this example is an even worse result.
The state of air pollution in London (after the events of 1952) came into extreme focus and four years later the Clean Air Act was passed by the British government. The act restricted burning of coal in both industrial furnaces and domestic fires and established “smoke-free” regions throughout the city. Residents were provided the option to change to heating sources like natural gas and electricity.
The Clean Air Act continues to be deemed a major event, “victory” if you will for residents and their health, in environmentalism for Britain.
Today, COPD is still vastly underdiagnosed.
If you or someone you know are looking for a resource, The American Lung Association has its’ “Better Breathers Club,” which connects persons living with COPD. For the past 40 years it has offered support and education throughout the country.
In positive momentum, an international team of researchers led by Michigan Medicine produced a “landmark study” which was funded by the National Heart, Lung, and Blood Institute.
The study reported a new diagnostic technique called Parametric Response Mapping (PRM) which is able to “identify small airway abnormality in COPD.”**** With better identification of problem areas, better treatment is allowed.
PRM “provides a color map, which represents normal lung tissue, small airway disease, or emphysema, and gives insight into the extent and localization of disease.”*****
A chart within this blog depicts PRM mapping. From left to right, normal lung tissue; small airway disease; and emphysema.
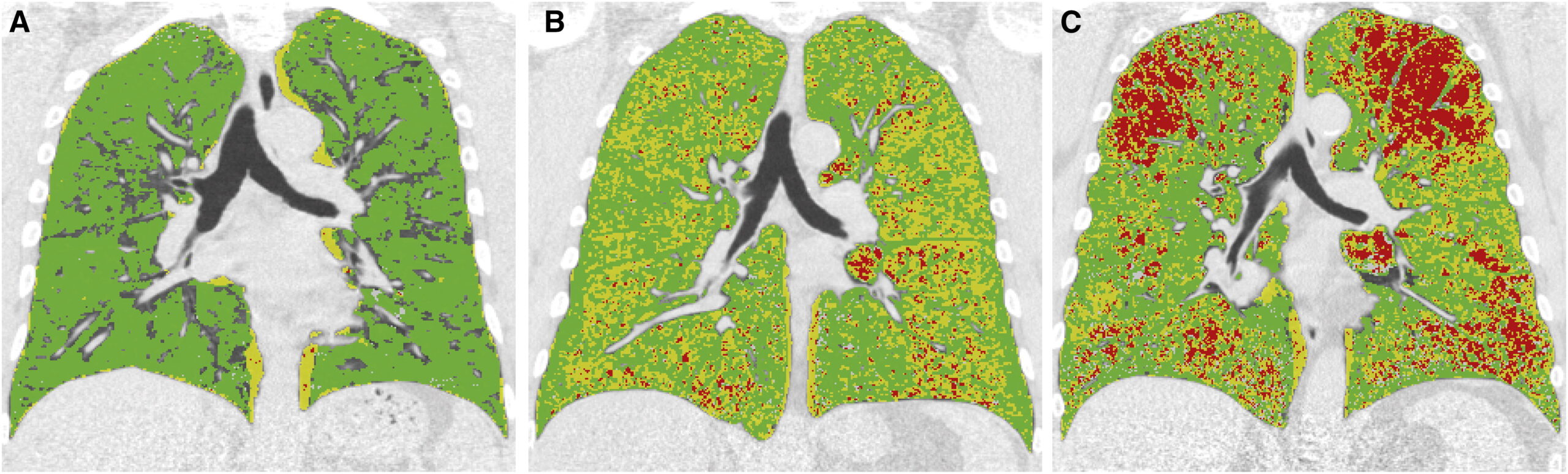
“PRM adds significantly to the diagnostic value of current CT quantification methods in assessing the presence of COPD.” Further investigation is anticipated.
When patients are diagnosed with COPD, they should be advised which of four “stages” their disease is in. This is based on what is known as the GOLD system for grading COPD. Determining which of the four stages pertains to the patient is based on things such as: magnitude of symptoms, how many times the COPD has escalated, and results of a spirometry test (checks the amount of air and speed the patient can exhale).
STAGE 1: Mild COPD – Lung capacity is estimated to be around 80 percent of normal. Moderate to persistent coughing and small amounts of sputum (saliva mixed with mucus) may be present.
STAGE 2: Moderate COPD – At this stage, the patient’s lungs are operating at between 50 and 80 percent. Coughing and the production of sputum are more prominent in these patients. These individuals will find they experience shortness of breath even with mild activity. It is at this stage that many people begin to seek a medical opinion.
STAGE 3: Severe COPD – Lungs are only operating at between 30 and 50 percent in these patients. Symptoms of fatigue and shortness of breath become more serious at this stage. With greatly reduced airflow into the lungs, these patients are likely to experience flare-ups, where infections in the lungs happen and hospitalization results.
STAGE 4: Very Severe COPD – Quality of life is very difficult for patients with Stage 4 COPD. With lung function at approx. 30 percent of normal, the disease becomes life-threatening. The accompanying coughing and mucus production becomes extremely complicated as it becomes increasingly difficult for the patient to clear their lungs of the mucus. Morning headaches can plague these patients who have higher levels of carbon dioxide in their blood and due to the stress on the heart, the feet can begin to swell.
If you or a family member or friend appear to be experiencing early signs of this disease, prompt medical attention is encouraged. The sooner the disease can be treated and managed, the better off the patient will be.
It is important to note that COPD and asthma are two completely different diseases. A thorough exam and evaluation by a pulmonologist can result in the proper diagnosis.
**Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2094286/pdf/1026.pdf
***Source: https://www.history.com/news/the-killer-fog-that-blanketed-london-60-years-ago
****Source: https://www.uofmhealth.org/news/archive/201903/non-invasive-imaging-technique-valid-identifying-small
*****Source: https://www.atsjournals.org/doi/10.1164/rccm.201411-2105LE
Coming next: Chronic illness can be invisible, cause aerobic impairment
Please consider sharing this article with family, friends, neighbors, coworkers. Let’s help each other reach optimal health.
