We all know what “snow” is on a television screen when a satellite or cable connection is lost, right? Imagine that happening to your vision.
Visual Snow and Visual Snow Syndrome, conditions that are under-represented and under-diagnosed, are still being heavily researched, but have been connected to migraine, concussions, infections, and serious brain and eye disorders.
To educate us more on this medical condition, I interviewed Dr. Francesca Puledda, a neurologist and post-doctoral researcher at King’s College in London.
Dr. Puledda’s background is in headache disorders. Visual snow syndrome is a condition in which she is very passionate about. In addition to being well-published, she has been involved in headache research since 2010.
Dr. Puledda said the best way to explain and gain an understanding of visual snow is based on patients’ reports of experiencing it. How the symptoms present themselves to each individual can vary.
Knowing this, it underscored why it is so important to consider any unusual experience like this to be valid to investigate. As we know with “invisible illnesses,” it can be difficult for others to understand or acknowledge them. This is particularly true if medical research and clinical data is not yet ample or been wide-reaching in awareness, as is true with Visual Snow Syndrome.
Dr. Puledda said patients “describe [visual snow] as these tiny flickering dots that kind of resemble, if you remember, the old analog televisions when they’re detuned.”
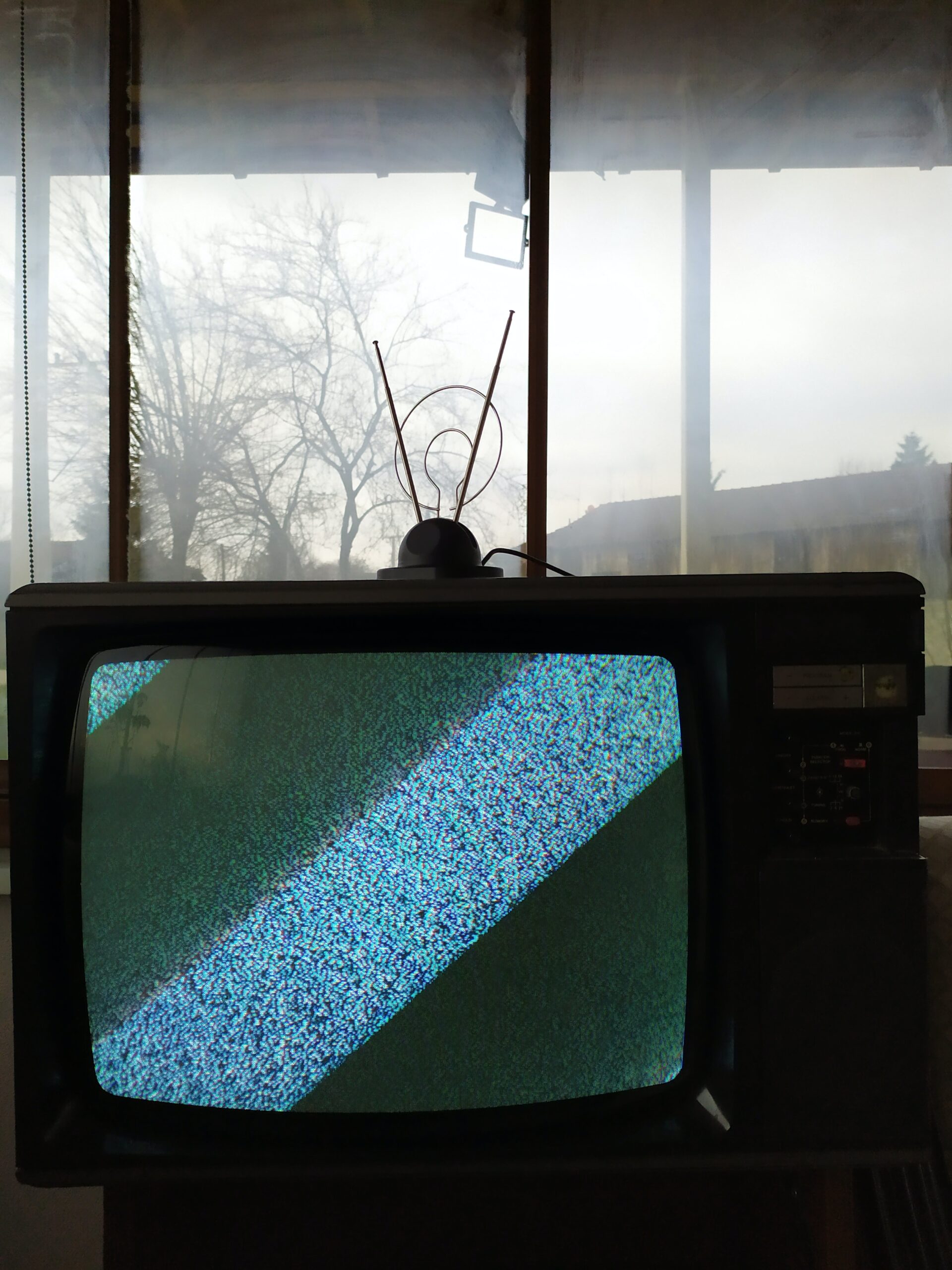
Essentially, patients “see this thick layer of static in front of their vision that covers pretty much every object that they look at.”
Visual Snow is “in their entire field of vision and constantly there,” she said.
While “static” is the primary symptom of it, Dr. Puledda explained that “we know Visual Snow Syndrome is a bit more complex than having simple static.”
“In fact, patients have several other symptoms that are caused by the brain but that manifest as visual phenomena,” she continued.
Dr. Puledda identified symptoms of visual phenomena, which include:
- Palinopsia – “They might look at an object, they look away, [and] the object is still in their vision, even if it’s not technically there.”
- Light sensitivity – “They have a very intense sensitivity to bright lights – even sunlight.”
- Nyctalopia – “They can’t really see well at night.” This tends to be “because their visual static is much more noticeable with low light.” She went on to say that it’s understandable “extreme light conditions – bright lights and low lights – are very difficult to endure.”
- Entoptic phenomena – Something many of us are familiar with – having “floaters” once in a while. She said that for people who experience visual snow floaters, “They are very frequent, really disruptive in their vision, [and] are very obvious.”
The good news about Visual Snow Syndrome is that it “does not cause problems to the brain and eyes; rather, it’s produced by the brain,” said Dr. Puledda.
Simply put and with more research needed to gain better clarity from a medical standpoint, “It’s a wrong way of processing normal visual information that comes from the outside,” she said.
As with any concerning symptoms, it can be beneficial to seek medical advice. When I inquired if tests or diagnostics can confirm Visual Snow Syndrome, Dr. Puledda said, “Essentially the diagnosis of Visual Snow is clinical.” What this means is, “We base it on the description of what the [patient] actually reports and the exclusion of secondary causes.”
Clinical criteria for Visual Snow was defined by a seminal publication in 2014.*
The clinical criteria allows a medical provider to “define if a patient is experiencing [one type of] visual snow or if they have a more complex form of Visual Snow Syndrome based on how many of the additional symptoms they have.”
While there is no “test” to diagnose Visual Snow, Dr. Puledda said, “It is very important to exclude any other conditions of either the brain or eyes that might mimic Visual Snow.”

This is due to the reality that medical providers “know there are very serious brain and eye disorders that can manifest with symptoms that are similar to Visual Snow,” she said.
What can a patient expect when they see a doctor about visual snow?
“We usually do a full neurological examination,” said Dr. Puledda. “We request a full eye examination with very in-depth tests, visual acuity, the visual fields, [and] also the visual fundus is very important to exclude any optic nerve issues.”
“Finally we usually request something that is called OCT (optical coherence tomography), which looks at the layers of the retina,” she said. “This is to confirm no other issues [exist].”
Dr. Puledda advised that each patient is different and it is wise to follow the steps and requests the physician makes.
For some patients, it may involve additional tests. “[There are patients who] may have other neurological symptoms that don’t quite fit Visual Snow, so we tend to also request brain imaging, MRI.”
As with many medical conditions, secondary conditions or a co-mingling of health factors are quite common.
Dr. Puledda said that tinnitus (ringing/buzzing in ears) and migraine often occur in patients who experience Visual Snow. “You don’t have to have [tinnitus and migraine] to experience Visual Snow,” she said. “But it very often happens together – concomitantly.”
I was curious if there was a common age that Visual Snow Syndrome appears in patients.
“This is a really difficult question to answer because I have to say that we don’t know enough about Visual Snow to know this for certain,” Dr. Puledda explained some initial findings from a study in which over 1,000 patients with Visual Snow were interviewed. “The subjects were quite young, the mean age was around 30, [yet] their visual snow had started much before that.”
“A large group in this cohort said they had always suffered from Visual Snow and they just realized it was something abnormal later in life,” she said. This underscored to me why seeking medical advice is so important, especially concerning these unique and under-represented conditions.
Dr. Puledda said there may be a spectrum of Visual Snow conditions, meaning people of all ages can have the condition and have it in different severities. “Obviously the ones that have more severe symptoms tend to come to us and approach us through the Internet, so that may be why our population is a bit biased to a younger age and with more severe symptoms,” she said.
For all its good points as well as challenges, this is an instance where the Internet has allowed a positive, progressive outlet for a better doctor/patient connection. Those who lived with Visual Snow before social media and Internet accessibility was mainstream clearly may have just kept it to themselves.
I think many of us are curious about where the root cause lies with many illnesses.
While research has not yet confirmed what leads to Visual Snow or what can lead to it, Dr. Puledda said, “It’s very likely that there is some form of genetic susceptibility to developing Visual Snow.”
Unfortunately, at this time, no study is looking in-depth at the link between genetics and Visual Snow.
Though, “There are illnesses that are connected to [visual snow] – the most important one is migraine,” Dr. Puledda said.
Many in the chronic illness community know how commonly “triggers” come into play. If you’re new to the term, a trigger, for example, is an event that can bring on a migraine attack.
“Some people have always had Visual Snow but [others], about a quarter of people with Visual Snow, just have it start one day and last until the next and we found that quite often it happens with migraine,” she said.
There does not seem to be an established pattern, but Dr. Puledda said, “Sometimes we see that when the Visual Snow starts, it starts with a migraine attack.”
Dr. Puledda said a paper** written by Dr. Carrie Beth Robertson “found several illnesses associated as a trigger to Visual Snow with the start of the condition.” Migraine was one and others included mild concussion and infection.
“There are several things that can start Visual Snow, but that isn’t to say that those are the causes,” Dr. Puledda said.
This is, of course, due to the fact of the great numbers of individuals who have experienced concussions or illnesses that have never developed Visual Snow.
“That’s possibly where the genetic / the congenital predisposition comes in,” she noted.
Visual Snow sufferers have been tapping into online information and it’s proving beneficial. “Having a diagnosis and recognition of what they have is extremely important,” Dr. Puledda said.
While she has advised that those who experience Visual Snow should seek medical attention, she said, “It’s quite normal that a lot of my colleagues don’t know what [Visual Snow] is [as] it’s fairly new, and has been given a name [only] very recently.”
“It’s not taught in medical school,” she said. And, “It’s not really necessarily anyone’s fault, but it’s a subjective disorder that is based on a recollection of an experience of a perceptual disorder.”
Visual Snow “is difficult to recognize and to diagnose,” Dr. Puledda confirmed.
Currently there is not a single drug that is known to be effective for the large majority of the population, she said. So, in her practice, it’s common to take a different approach to treatment. This is by “either try[ing] to take care of secondary illnesses (migraine/anxiety or low mood) that are perhaps going on with the Visual Snow (not causing it), but they might be going together, so perhaps working on one can help the other.”
Dr. Puledda said she has gathered some helpful tips from patients and others regarding visual snow, which include:
- Learning coping mechanisms – This “could help them work on the stress related to the symptoms. That takes some time and sometimes it takes professional psychological help, but often it can help to take the attention away.”
- Working on brain intentional mechanisms – Since they “are altered in Visual Snow.”
- Partaking in meditation or cognitive behavioral therapy.
- Wearing tinted lenses – “Especially on the yellow/blue spectrum, especially [beneficial] with sensitivity to light.”
She said there “are several options and I think they need to be discussed on an individual basis with a medical professional.”
When asked what she feels is the most under-represented condition in neurology, Dr. Puledda said, “In general, all the conditions that can’t really be measured by a single specific test (like blood pressure/blood sugar), [that] tend to be very under-represented.”
“Generally, conditions that are subjective and don’t really show externally tend to be under-diagnosed and under-represented in funding and research and even attention given to it in medical school,” Dr. Puledda said.
She said she has admiration for patients that are having to live with Visual Snow. “It’s been an incredible journey to see how dedicated people are to help with research and help with understanding their own condition and that is something quite unique to this patient group (it’s one of their main features),” Dr. Puledda noted.
A strong supporter of greater understanding of the condition, Dr. Puledda said, “It’s so important to share your medical experiences.”
As we know, our voices can make a difference in medical care.
Please consider sharing this article on Visual Snow in an effort to reach individuals experiencing it, those who are close to these individuals, and to bring more awareness to the need for more research into this condition.
*’Visual snow’ – a disorder distinct from persistent migraine aura. Christoph J. Schankin, Farooq H. Maniyar, Kathleen B. Digre, Peter J. Goadsby, Brain, Volume 137, Issue 5, May 2014, Pages 1419-1428. https://doi.org/10.1093/brain/awu050
**Mehta DG, Garza I, Robertson CE. Two hundred and forty-eight cases of visual snow: A review of potential inciting events and contributing comorbidities. Cephalalgia. 2021;41(9):1015-1026. doi:10.1177/0333102421996355
Please consider sharing this article with family, friends, neighbors, coworkers. Let’s help each other reach optimal health.
