The interview this month is with Dr. Payam Soltanzadeh, who specializes in neurology and neuromuscular medicine at University of California Los Angeles (UCLA). Dr. Soltanzadeh has shared his expertise and provided clarity on the condition Myasthenia Gravis (MG).
“In Myasthenia Gravis, what happens is antibodies attack the junction between the nerve and muscle,” Soltanzadeh explained. A helpful comparison is when a person has trouble with their thyroid, i.e., “the antibodies attack the thyroid.”
“In Myasthenia Gravis the connection between the nerve and muscle is disrupted and because of the disruption of the receptors (the signals/molecules that are secreted from the nerve), the connection between the nerve and muscle is not as efficient,” Soltanzadeh detailed. Individuals “have a lot of reserve, but people who develop the symptoms [of the disease], pass that threshold and develop easy fatigability.”
While Myasthenia Gravis “doesn’t respect any ages,” Soltanzadeh explained that the condition is seen in two predominate age groups. “In ladies, it’s usually under [age] 40 and in men it’s usually after [age] 60.” While less common, it can and does affect children and teenagers, Soltanzadeh said.
Statistically speaking, between “40,000 and 60,000 people are thought to have Myasthenia Gravis in the United States,” Soltanzadeh said. This is with the caveat that “it’s also underdiagnosed.” He explained that if a person “has very mild ocular Myasthenia Gravis, they may not even seek attention if they are not paying much attention to it (this includes having droopy eyelids).” As statistics are prone to bias, these are the numbers currently sourced and relied upon.
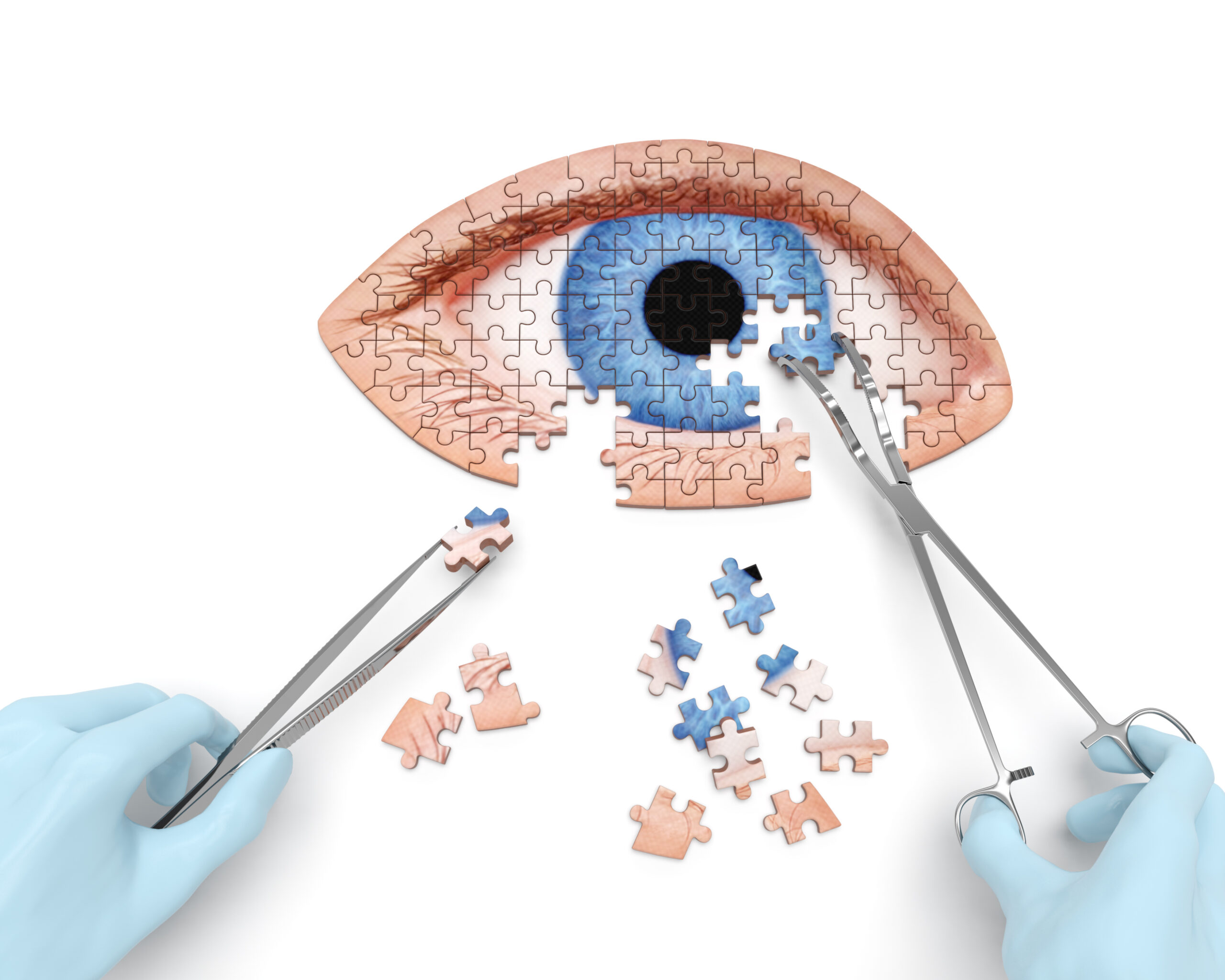
Nearly everyone with the disease will have two of the most common symptoms appear in the first couple of years, “droopy eyes and trouble with eye movements,” Soltanzadeh said. In addition, “[a patient] may also get problems with muscles that are involved in swallowing and talking.”
Some Myasthenia Gravis patients may suffer from only what is called “Ocular Myasthenia.” In “Ocular Myasthenia Gravis” or “eye Myasthenia Gravis,” “the condition remains only in the eyes and it doesn’t generalize, it doesn’t go beyond the eyes,” he explained. About 50% of patients with Ocular Myasthenia progress to generalized Myasthenia in a couple years.
When Myasthenia Gravis goes beyond the eyes, it can impact the muscles of articulation and swallowing. Persons with Myasthenia Gravis may slur their speech or have difficulty consuming liquids or foods. For most patients, the afternoon and evening time frames prove to be the most difficult. When caring for a Myasthenia Gravis patient, it’s important to remember that mornings may be easier for them, but by the end of the day, they may need help with physical tasks and also appreciate emotional support.
While the eyes and throat contain the most common muscles affected, it is important to note that all the muscles in the body can be affected by Myasthenia Gravis. Some patients may experience muscle weakness in the legs and arms. The key here is follow up, he said, because “we can not predict [what the disease is going to do] very well.”
My late grandmother had Myasthenia Gravis and experienced facial weakness, trouble breathing, and droopy eyelids. I recall she was treated in part with a drug called Mestinon and Prednisone and did experience side effects. The medications did allow her to lead a more normal life though.
Soltanzadeh said diagnosing Myasthenia Gravis includes “observing the patient” in an examination and understanding a patient’s medical and family history. “Like anything in medicine, the history is important,” he said, especially when a patient tells him about droopy eyelids, issues with vision – double vision, trouble driving. An in-office exam of a patient’s eye movements is part of the initial examination as well as observing if a patient is having a tough time opening their eyes or have weak jaw muscles.
Compared to the 1960s when confirming that a person has Myasthenia Gravis was much more difficult, present day it is much easier and more definite as a blood test confirms it in most cases. “The most helpful way [to accurately diagnose the disease] is having a positive antibody,” said Soltanzadeh. “In about 90% or more of our patients, they have antibodies.”
Myasthenia Gravis can also be determined by electro-diagnostic ways (EMG). Soltanzadeh explained, “In the electro diagnostic lab we repeatedly stimulate the nerve and see if the amount of response we are getting from the muscle shows a significant decline (a decrement).”
In addition to fitting into one of the age categories Soltanzadeh identified “having a personal history of autoimmune disease is probably the number one risk factor” for developing Myasthenia Gravis.
You may be curious how family history plays a part in acquiring the disease. I certainly was, as my late grandmother was diagnosed at the age of 64. Soltanzadeh said, “If there is family history, there are some statistics of up to three percent” for relatives to acquire the disease.
There are myriad treatment and management options for Myasthenia Gravis patients. Two main categories are symptomatic treatment and immune modulatory treatment. Symptomatic treatment’s goal is “to make this connection [between the nerves and muscles] better – to kind of ‘boost the connection.’” One common medication is Mestinon and “that may be in some cases the only medication [a patient] needs (perhaps in Ocular Myasthenia Gravis),” Soltanzadeh said. This is how my grandmother was successfully treated.
Medications that boost the nerve/muscle connection “allow more signal molecules to stick around the junction of the nerve and muscle and help bring more signal to the muscle in order for the muscle to be able to contract,” Soltanzadeh noted.
“Suppress[ing] or modulat[ing] the immune system is the main treatment to suppress the disease because it’s an autoimmune disease,” Soltanzadeh explained. This, in turn, weakens a person’s immune system, “so the body has a better chance to recuperate from the damage.”
Some corticosteroids, such as the widely known Prednisone, is a common treatment option. Soltanzadeh explained that Prednisone “has to be tailored over time. It’s a very delicate route. It comes with a lot of side effects so it has to be tailored to the needs [of a patient].” My grandmother endured various adjustments as the Prednisone caused noticeable “puffiness” in her body.
Patients may also be given a steroid-sparing medication that also suppress the immune system like Imuran or CellCept.
Soltanzadeh explained that in tailoring medication for a Myasthenia Gravis patient, the goal is “to have the immune system at a level to have [the disease] controlled but also you’re not completely shutting down the immune system.” This is so the body can “defend itself against infections, cancer and so forth.”
For a severe Myasthenia Gravis patient that has trouble breathing and is very ill, an immune modulatory treatment, such as intravenous immunoglobin (IVIG) might be used.
“Another main treatment, if indicated, is removal of thymus gland or thymectomy,” Soltanzadeh explained. This is because “the thymus is a major factory of cells of the immune system and they have shown that in most patients with Myasthenia Gravis removal of the thymus can help modulate the immune system in a way that would help them.”
Supportive treatments can include prescribing a patient glasses if they have double vision. A patient “may benefit from prisms,” Soltanzadeh said.
Migraine isn’t directly linked to Myasthenia Gravis. Though Soltanzadeh explained that “eye strain is a well known cause of headache” and people with Myasthenia Gravis “kind of struggle with focusing on the target; they see double, and the eyes droop, and they are trying to see one instead of two.” This, in turn, “definitely can be a factor causing worsening of [a patient’s independent] headache.”
In addition, Soltanzadeh said, “if [a Myasthenia Gravis patient is] fatigued or if they are not drinking enough water and they are dehydrated, those things can secondarily aggravate or make them prone to more attacks of migraine or headache.” He also noted that patients who have weakness in the throat muscles or sleep apnea, “may get morning headaches.”
As we know, every chronic condition is different and the physical and emotional tolls surely fluctuate person to person. Supporting a Myasthenia Gravis patient is extremely important.
First and foremost, educating yourself about the disease is important. Understanding the symptoms, the challenges, the medical treatment options and how you, your loved one, or the individual you are providing care for is vital.
Soltanzadeh said loved ones and caregivers should “always offer help [to the patient, depending on your relationship to them]” and “be with them as much as you can.”
“Just being there so they know you are there to help” is immensely beneficial, he added.
Family members should be mindful that as the day progresses, Myasthenia Gravis patients can struggle more with the disease. Offering help with physical tasks would be helpful, because patients may have a limited reserve for doing physical activities and get exhausted sooner.
And of course, “show love to them so they feel like they are not left alone,” he said. As with many chronic conditions and diseases “emotional and psychological consequences are very important.”
Soltanzadeh said Myasthenia Gravis patients can develop “very significant secondary fatigue, which is different from Myasthenia Gravis fatigue, and usually may come with a lot of anxiety and stress.”
In addition to emotional and physical help, being a supportive family, friend, or caregiver by ensuring that the Myasthenia Gravis patient is getting regular medical checkups is vital.
The Myasthenia Gravis Foundation of America offers plentiful resources to understand all aspects of Myasthenia Gravis. https://myasthenia.org/
Coming next: Emotional intelligence helps guide solution-based thinking
Please consider sharing this article with family, friends, neighbors, coworkers. Let’s help each other reach optimal health.